Undergraduate Medical Education (UGME) at McMaster
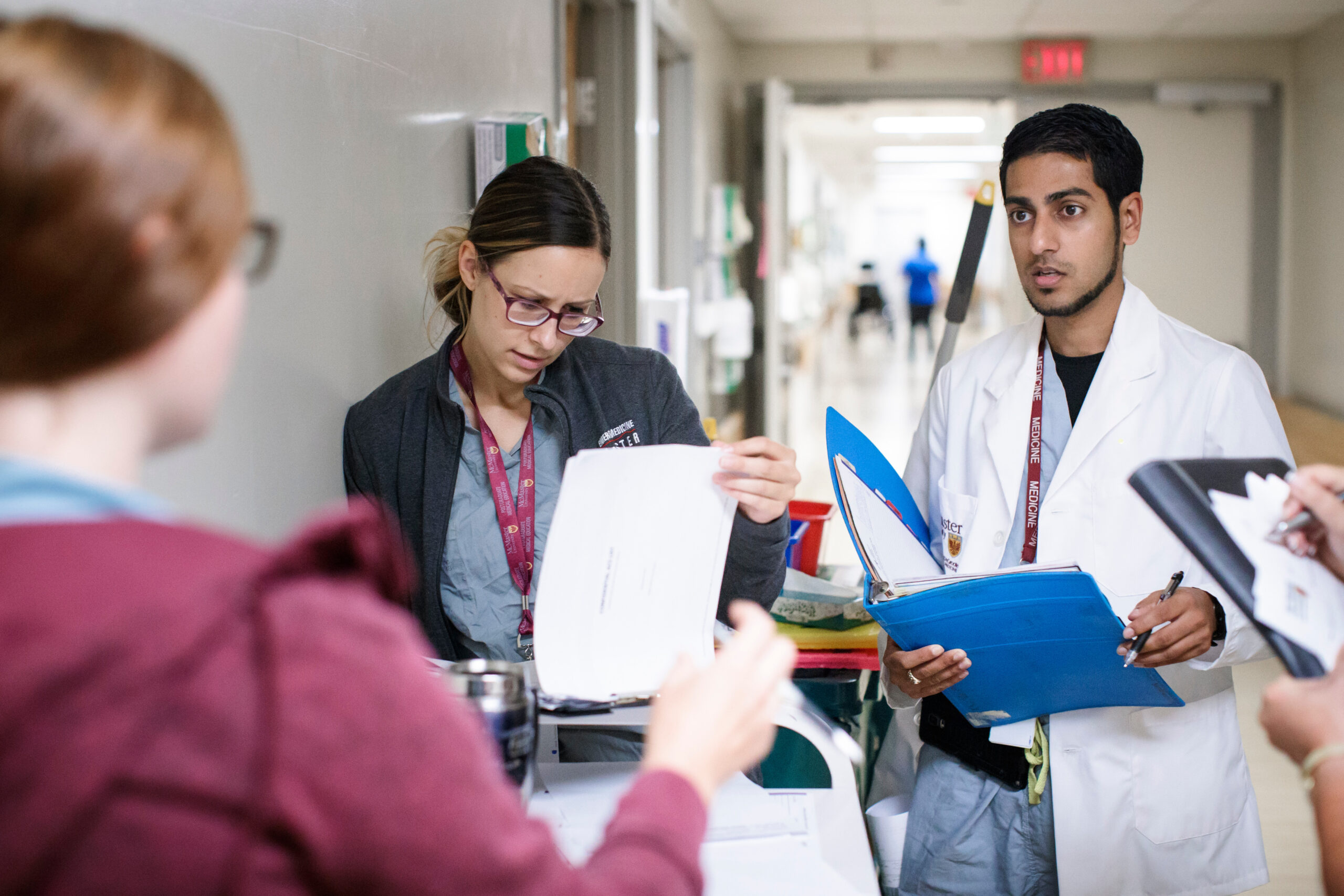
The UGME program’s mission is to educate and inspire future physicians to improve health and well-being for all through clinical excellence, innovation, scholarship, leadership, and social accountability.
The UGME program at McMaster University is known worldwide for its innovative approach to medical education, including problem-based learning, early clinical exposure, and three-year curriculum delivered within a distributed medical education model. Our reach and impact are impressive, with over 4,000 faculty spread across two distributed campuses and four clinical education campuses in Southwestern Ontario.